 To continue fromwhere we left off in the previous post (you may want to go back and read that
if you haven’t) let’s look at another evolutionary arguments for the importance
of our microbiome. Bacteria have been colonising humans since we first
existed. Human eating habits have changed a lot within a very short period.
Throughout much of our evolutionary time we have eaten a diet ripe in bacteria
– meat caught and slaughtered outside, vegetables grown naturally in fields and
so on. However, within recent times our food production (and consumption) has
changed. Processed foods have become increasingly common, and these are largely
sterile. Additionally, antibiotics are heavily used in the animal farming industry;
reducing the amount of bacteria we receive from our food. Some claim that this
may be disrupting our microbiome, as we are not getting the same level and
diversity of bacteria. Furthermore, this disruption caused by out eating habits may be
playing a role in the development of obesity in the Western world. Obviously
the diet itself plays a major role in obesity, but the microbiome may also
contribute. Consider the fact that if we have a gut full of bacterial cells all
needing energy, they are going to take what they need from the food we ingest,
before we absorb it for ourselves. If we have less microbes, in the gut, and
less coming in with our food, then less energy will be taken out of the system,
potentially allowing more to enter into our bodies; this excess of energy may
well be play a significant role in obesity.
To continue fromwhere we left off in the previous post (you may want to go back and read that
if you haven’t) let’s look at another evolutionary arguments for the importance
of our microbiome. Bacteria have been colonising humans since we first
existed. Human eating habits have changed a lot within a very short period.
Throughout much of our evolutionary time we have eaten a diet ripe in bacteria
– meat caught and slaughtered outside, vegetables grown naturally in fields and
so on. However, within recent times our food production (and consumption) has
changed. Processed foods have become increasingly common, and these are largely
sterile. Additionally, antibiotics are heavily used in the animal farming industry;
reducing the amount of bacteria we receive from our food. Some claim that this
may be disrupting our microbiome, as we are not getting the same level and
diversity of bacteria. Furthermore, this disruption caused by out eating habits may be
playing a role in the development of obesity in the Western world. Obviously
the diet itself plays a major role in obesity, but the microbiome may also
contribute. Consider the fact that if we have a gut full of bacterial cells all
needing energy, they are going to take what they need from the food we ingest,
before we absorb it for ourselves. If we have less microbes, in the gut, and
less coming in with our food, then less energy will be taken out of the system,
potentially allowing more to enter into our bodies; this excess of energy may
well be play a significant role in obesity.
The use of
antibiotics by farmers also argues for a role of the microbiome in obesity. The
reason antibiotics are used by farmers is from the observation that this practice
caused a gain of weight in the animals. For a long time this was not
understood, but now with the evidence emerging from humans and other animal
studies it appears that this affect could be down to the depletion of the microbiome
caused by the antibiotics. A further example comes from studies in mice which have shown that transplanting the microbiome from an obese mouse into a thin
mouse leads to weight gain. The reverse has also been seen. If this holds true
in humans then targeting the microbiome may be a feasible way to tackle the obesity
epidemic of the Western world.
Changing tack slightly, as you may be
aware, antibiotics have been overused for a long time, leading to major worries
over antibiotic resistance and reversion to a pre-antibiotic era. This is a huge
worry, however the overuse of antibiotics may have additional consequences that
we are only just starting to realise. It has been found that people in the
Western world are now largely devoid of the bacterium Helicobacter pylori,
which is common in the guts of people in areas of the world less rife in the use of
antibiotics. Removal of H. pylori isn't a bad thing per se; this bacterium is
known to cause peptic ulcers and stomach cancer. However, the importance of H.
pylori is a nice shade of grey and we have only noticed the beneficial effects
now it’s gone.
H. pylori plays
an important role in controlling stomach acid production and people devoid of
it are at a much higher risk of developing acid reflux. Acid reflux can lead to
a condition known as Barrett's oesophagus and eventually certain forms of
oesophageal cancer if left untreated. Coincidently with the loss of H. pylori
from the gut microbiome in the West, rates of oesophageal cancer have soared. Furthermore,
H. pylori is able to control inflammatory responses. This control may be
important for regulating allergies, which are caused by an inappropriate
inflammatory response against something harmless (such as pollen).
Similarly to the rates of oesophageal cancer, it is well documented that there
are an increasing number of people with allergies in the Western world. Finally, H. pylori may also be important in obesity, as it is known to regulate the
hormone ghrelin, which regulates our appetite. All of this has led to some suggestions
that we should inoculate babies with H. pylori. Obviously this raises
ethical issues because of the potential for peptic ulcers and stomach cancer,
but these are largely only seen later in life. The current idea is that we should
inoculate at a young age and then give antibiotics to kill the bacteria later in
life, getting the best of both worlds.
A mentioned, H.
pylori may be playing a role in the inflammatory response and development of
allergies. However, the link between resident bacteria and the immune system
doesn’t end there. It appears that our whole microbiome is essential for the
development of a proper immune system that doesn't attack the wrong things. Without
the bacteria in our guts it is thought that the immune system may become hypersensitive
and attack everything, leading to allergies.
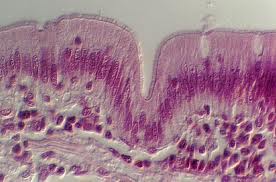 |
| Histological section of intestine lining |
Sticking with
the immune system, many chronic diseases have inflammation as an underlying
cause. Inflammation is an essential part of our immune response, but is only
beneficial if it is transient; sustained inflammation leads to damage around
the body. It has been found that Bifidobacteria and Lactobacilus species in the
gut are essential for maintenance of the epithelial lining in this organ (the
cells that make up the walls of our gut). A proper epithelial lining plays an
essential role in the passage of nutrients out of our digestive system into our
blood. The lining needs to be ‘selectively permeable’ so that only certain,
useful, things get through. If the lining becomes ‘leaky’, then unwanted
molecules can get through such as bacteria and their toxins or whole protein
molecules (instead of just the amino acids we normally absorb from the gut),
all of which could trigger an inappropriate immune response. Since
Bifidobacteria and Lactobacilus are needed for maintenance of the epithelial
lining, any disruption to these bacteria will have an impact on the integrity
of the barrier. Indeed, it has been shown that mice fed on a "junk
food" diet have a disruption of these bacteria and develop a ‘leaky
epithelia’. This caused a low level systemic inflammatory response, which
eventually causes metabolic diseases. It is therefore highly possible that many
disease with inflammation as an underlying cause could originate from issues
with out internal bacterial species.
 The final thing
I'd like to discuss is that the notion of thinking with your gut may hold more
truth than you know. It has been found that microbes in the gut are important
for the generation of neurotransmitter molecules such as serotonin and thus may
be playing an important role in regulating mood. Furthermore, there is evidence
suggesting a link between the gut microbiome and the hypothalamic-pituitary
axis (HPA), a region of the brain that shows disruption during clinical
depressive episodes. Mice bred to have no microbiome show an enhanced stress
response that can be curtailed by the introduction of a microbiome - this
response, to a large extent, is generated from the HPA. Additionally, it been
shown in mice that if the microbiome of adventurous mice is transplanted into
the guts of timid mice they lose their inhibitions and become more adventurous,
further supporting the notion that our gut bacteria may be influencing our
brains.
The final thing
I'd like to discuss is that the notion of thinking with your gut may hold more
truth than you know. It has been found that microbes in the gut are important
for the generation of neurotransmitter molecules such as serotonin and thus may
be playing an important role in regulating mood. Furthermore, there is evidence
suggesting a link between the gut microbiome and the hypothalamic-pituitary
axis (HPA), a region of the brain that shows disruption during clinical
depressive episodes. Mice bred to have no microbiome show an enhanced stress
response that can be curtailed by the introduction of a microbiome - this
response, to a large extent, is generated from the HPA. Additionally, it been
shown in mice that if the microbiome of adventurous mice is transplanted into
the guts of timid mice they lose their inhibitions and become more adventurous,
further supporting the notion that our gut bacteria may be influencing our
brains.

